SOMANZ Poster Presentation Australasian Diabetes in Pregnancy Society and Society of Obstetric Medicine Australia and New Zealand Joint Scientific Meeting 2025
Biopsy-confirmed, seronegative PLA2R-positive primary membranous nephropathy in a dichorionic diamniotic twin pregnancy managed with rituximab. (#163)
Primary membranous nephropathy (PMN) in pregnancy poses significant risks, including; preeclampsia, preterm delivery, low birth weight, and fetal death. Majority of PMN cases are associated with circulating anti-PLA2R antibodies, aiding diagnosis and management.
We report a case of seronegative but renal biopsy PLA2R-positive PMN in a 27-year-old Caucasian multigravida (G3P1) with a dichorionic diamniotic twin pregnancy. She exhibited persistent hypoalbuminaemia (15 g/L at 20+6 weeks) and nephrotic-range proteinuria (urine PCR 1413 mg/mmol at 28+1 weeks), while remaining normotensive with preserved renal function. Prednisolone (60mg daily) was initiated at 21 weeks due to concern for lupus nephritis (ANA 1:640, Ro-positive, La-negative). Secondary causes were excluded (negative ANCA; ENA; anti-dsDNA; normal C3/C4; negative syphilis and hepatitis B at 21 weeks). Pre-eclampsia was clinically excluded, sFLT1:PIGF was normal.
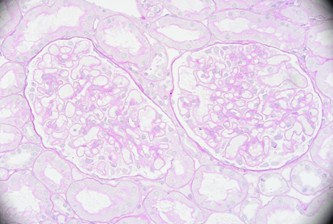
Renal biopsy at 27 weeks demonstrated subepithelial granular IgG, C3, and C1q deposition with PLA2R and IgG4 staining, confirming PMN. Serum PLA2R remained negative, consistent with early disease and intrarenal antibody sequestration.
She received rituximab 1g doses at 25+6 and 27+6 weeks, with a 6-week bridging course of tacrolimus and therapeutic enoxaparin. Proteinuria decreased to 500 mg/mmol and albumin improved to 22 g/L by 31+6 weeks. She delivered via emergency caesarean at 33+3 weeks following premature rupture of membranes. Twin 1 (1880g) and 2 (1925g) both had Apgars of 6, 8 and 9. By March 2025, she was in remission (albumin 32 g/L, urine ACR 7 mg/mmol).
This case underscores the diagnostic challenges of seronegative PMN and the potential role of rituximab in pregnancy.
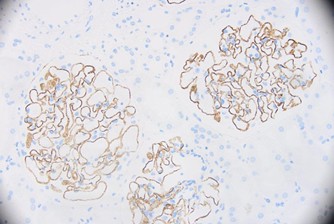
IgG4