SOMANZ Poster Presentation Australasian Diabetes in Pregnancy Society and Society of Obstetric Medicine Australia and New Zealand Joint Scientific Meeting 2025
Hypocholesterolaemia as an Early Marker of Acute Fatty Liver of Pregnancy: A Diagnostic Aid in Resource-Limited Settings (#160)
Introduction:
Acute fatty liver of pregnancy (AFLP) and HELLP syndrome share overlapping features, often complicating clinical differentiation. While both require expedited delivery, accurate distinction is critical for maternal risk assessment, neonatal outcomes, and future pregnancy planning. The Swansea criteria, though widely used, lack specificity, with many HELLP cases also meeting its diagnostic thresholds.1 Alternative biochemical markers such as hypocholesterolaemia, reduced antithrombin III and fibrinogen, and elevated soluble Fms-like tyrosine kinase-1 (sFLt-1) may provide improved accuracy over the Swansea criteria.2-4
Case Presentation:
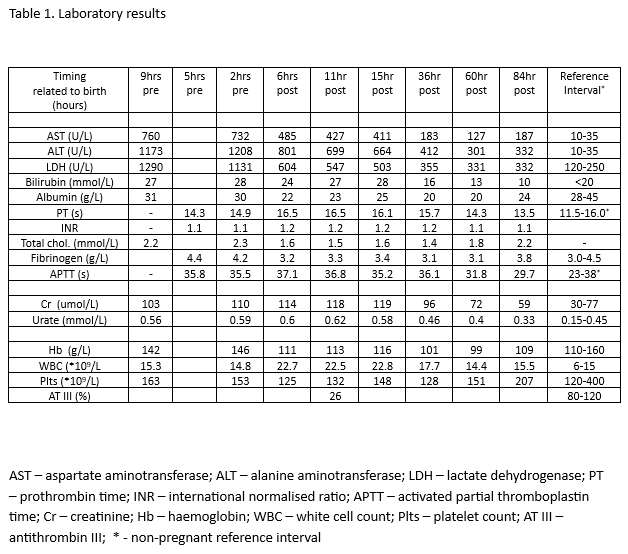
A 31-year-old primigravida at 37 weeks presented with hypertension, polyuria, hyperuricaemia, transaminitis, and acute kidney injury. She fulfilled six Swansea criteria but had profound hypocholesterolaemia (nadir 1.4 mmol/L) and low antithrombin III (26%). Labour was induced, resulting in vaginal delivery of a healthy male infant weighing 3000 g. Postpartum recovery was rapid, with normalization of hepatic and coagulation markers. Her pre-pregnancy cholesterol was 4.6 mmol/L, reinforcing that hypocholesterolaemia was an acquired pregnancy-related feature.
Discussion:
Physiological cholesterol elevation occurs in late pregnancy.5 Thus, marked hypocholesterolaemia may serve as an early sign of AFLP, preceding coagulopathy (Table 1). Retrospective reviews show consistently lower cholesterol in AFLP compared with HELLP.4,6-10 Additionally, low antithrombin III and elevated sFlt-1 may enhance diagnostic precision.2,4 Given cholesterol testing is widely available, its use—especially alongside antithrombin III—could improve bedside differentiation of AFLP from HELLP, particularly where advanced laboratory resources are limited.
Conclusion:
In resource-limited settings, profound hypocholesterolaemia may serve as an accessible, cost-effective diagnostic aid for AFLP, supporting early risk stratification in urgent obstetric scenarios.
- 1. Devarbhavi H, Venkatachala PR, Devamsh GN, et al. Swansea criteria evaluation in acute fatty liver of pregnancy, HELLP syndrome, pre-eclampsia, and viral acute liver failure in pregnancy. Int J Gynaecol Obstet. 2023;163(6):1030-2. doi:10.1002/ijgo.15137
- 2. Trottmann F, Raio L, Amylidi-Mohr S, et al. Soluble fms-like tyrosine kinase 1 (sFlt-1): A novel biochemical marker for acute fatty liver of pregnancy. Acta Obstet Gynecol Scand. 2021;100(10):1876-84. doi:10.1111/aogs.14218
- 3. Byrne JJ, Seasely A, Nelson DB, et al. Comparing acute fatty liver of pregnancy from HELLP syndrome. J Matern Fetal Neonatal Med. 2022;35(7):1352-62. doi:10.1080/14767058.2020.1754790
- 4. Vigil-De Gracia P. Acute fatty liver and HELLP syndrome: two distinct pregnancy disorders. Int J Gynaecol Obstet 2001; 73: 215-220. 2001/05/30. DOI: 10.1016/s0020-7292(01)00364-2.
- 5. Bartels A, Egan N, Broadhurst DI, et al. Maternal serum cholesterol levels are elevated from the first trimester of pregnancy: A cross-sectional study. J Obstet Gynaecol. 2012;32(8):747-52. doi:10.3109/01443615.2012.714017
- 6. Lamprecht A, Morton A, Laurie J, et al. Acute fatty liver of pregnancy and concomitant medical conditions: A review of cases at a quaternary obstetric hospital. Obstet Med. 2018;11(4):178-81. doi:10.1177/1753495X18764816
- 7. Cejudo Carranza E, Helguera Martinez A and Garcia Caceres E. [Acute fatty liver in pregnancy. Experience of 7 years]. Ginecol Obstet Mex 2000; 68: 191-197. 2000/07/21.
- 8. Lau HH, Chen YY, Huang JP, et al. Acute fatty liver of pregnancy in a Taiwanese tertiary care center: a retrospective review. Taiwan J Obstet Gynecol 2010; 49: 156-159. 2010/08/17. DOI: 10.1016/S1028-4559(10)60033-2.
- 9. Cheng N, Xiang T, Wu X, et al. Acute fatty liver of pregnancy: a retrospective study of 32 cases in South China. J Matern Fetal Neonatal Med 2014; 27: 1693-1697. 2013/12/07. DOI: 10.3109/14767058.2013.871704.
- 10. Nelson DB, Yost NP and Cunningham FG. Acute fatty liver of pregnancy: clinical outcomes and expected duration of recovery. Am J Obstet Gynecol 2013; 209: 456 e451-457. 2013/07/19. DOI: 10.1016/j.ajog.2013.07.006.