ADIPS Poster Presentation Australasian Diabetes in Pregnancy Society and Society of Obstetric Medicine Australia and New Zealand Joint Scientific Meeting 2025
Overt Diabetes in Pregnancy: Clinical Implications and Outcomes (#110)
Background:
We hypothesised that women with Overt Diabetes in pregnancy(ODM) have comparable risks of adverse outcomes to those with pre-gestational Type 2 diabetes(T2D).
Aim:
To compare the risk of adverse pregnancy outcomes in T2D, ODM and GDM.
Methods:
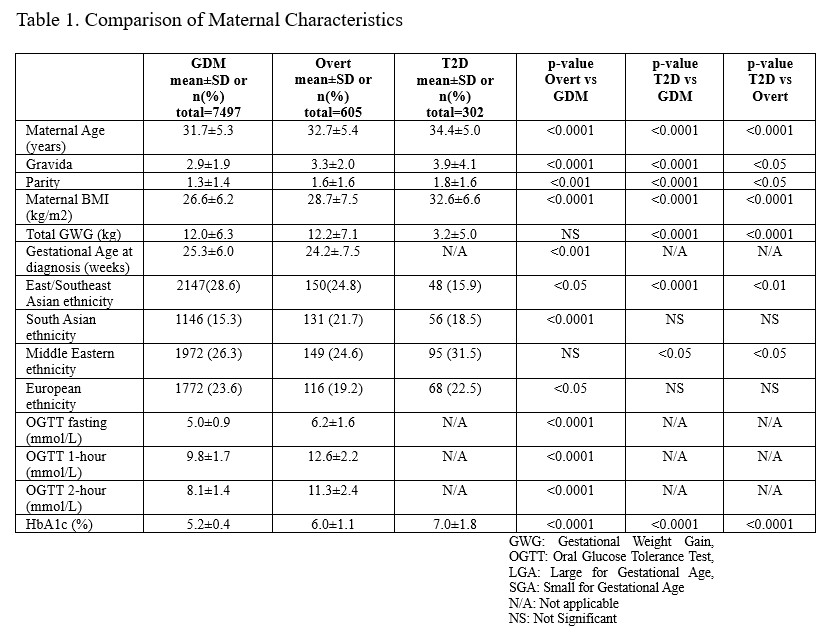
We analysed prospectively collected data from singleton pregnancies(1992–April 2025) involving GDM(n=7497), ODM(n=605), and T2D(n=302). ODM was defined as fasting glucose≥7.0 mmol/L, 2-hr≥11.1mmol/L(on OGTT), or HbA1c≥6.5%. Outcomes included insulin use, caesarean section(CS), preterm birth(<37 weeks), LGA, SGA, neonatal hypoglycaemia(NH), jaundice, and shoulder dystocia(ShD).
Results:
Compared to GDM, both ODM and T2D women had higher maternal age, gravida, parity(all p<0.0001). There were fewer East/South-East-Asian women among ODM and T2D compared to GDM(p<0.001 and <0.0001, respectively). Compared to ODM, T2D women had higher Maternal age(p<0.0001), pre-pregnancy BMI(p<0.0001), gravida(p<0.05), parity(p<0.05), with more Middle-Eastern women (p<0.05)-Table1.
Consistent with our previous study[1], many ODM women were normoglycaemic post-partum(46.4%).
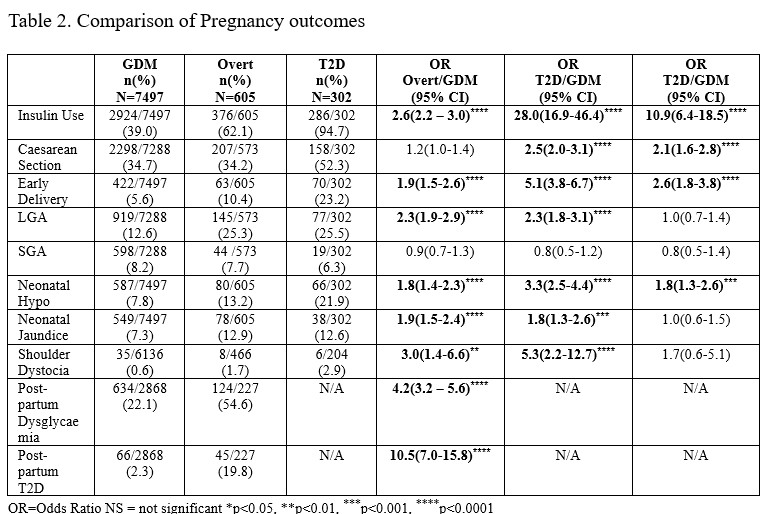
LGA was higher in ODM(25.3%), and T2D(25.5%) compared to GDM(12.6%) [both, p<0.0001]. Neonatal jaundice and ShD were higher in ODM(1.7%) and T2D(2.9%), compared to GDM(0.6%)[p<0.01and<0.0001, respectively]. There were no significant differences in LGA or ShD rates between T2D and ODM.
Insulin use, pre-term delivery, and NH were higher in T2D and ODM, compared to GDM(all p<0.0001), and significantly higher in T2D compared to ODM (p<0.0001,<0.001 and <0.0001, respectively)-Table2.
Conclusions:
ODM represents a state of intermediate risk between GDM and T2D regarding insulin use, pre-term delivery, CS and NH. Rates of LGA, neonatal jaundice and ShD are comparable between ODM and T2D. Hence ODM warrants similar surveillance to T2D.
- 1. Wong, T., et al., The clinical significance of overt diabetes in pregnancy.[Erratum appears in Diabet Med. 2013 Jul;30(7):887]. Diabetic Medicine, 2013. 30(4): p. 468-74.